So is transparency, and communication. When you pay for an outsourced partner, you deserve for them to care as much about your revenue as you do.If you feel like your claims aren’t being worked, then most likely they aren’t. If your insurance billing partner is giving you the runaround, most likely your AR is in trouble. If your partner isn't an expert in eyecare billing, perhaps your payments are slow for a reason.Set up an appointment with a Billing Expert:If your current partner isn’t...
John
From Our Resources
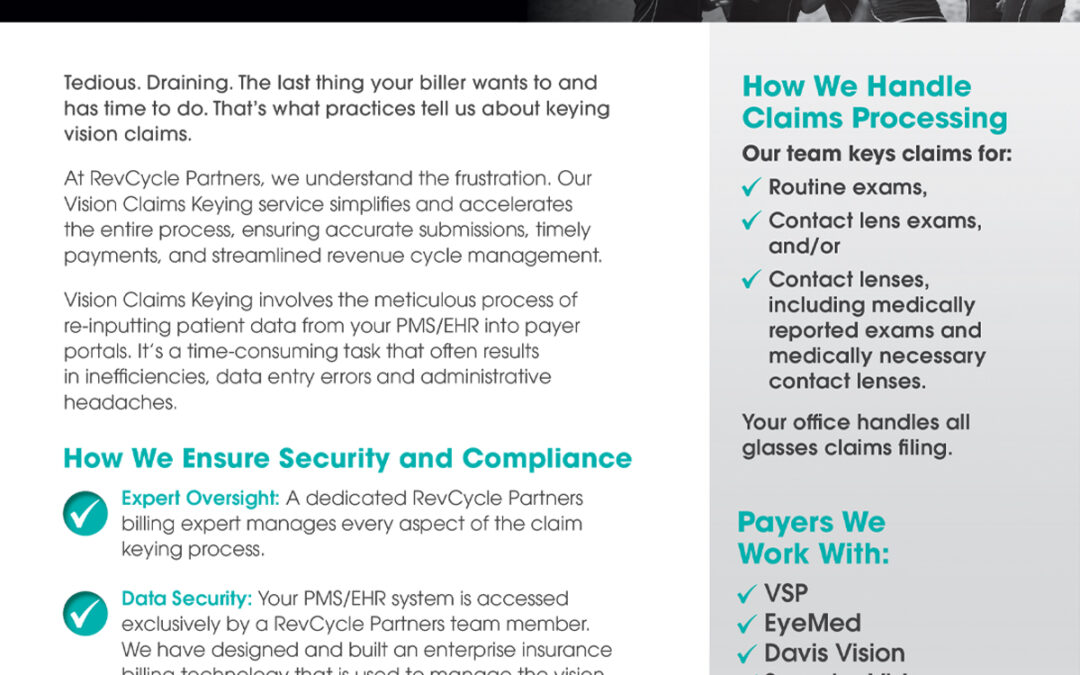
Vision Claims Keying
Vision Claims Keying - Find relief from the tedium of keying data. At RevCycle Partners, we understand the frustration. Our Vision Claims Keying service simplifies and accelerates the entire process, ensuring accurate submissions, timely payments, and streamlined revenue cycle management. Download the PDF »
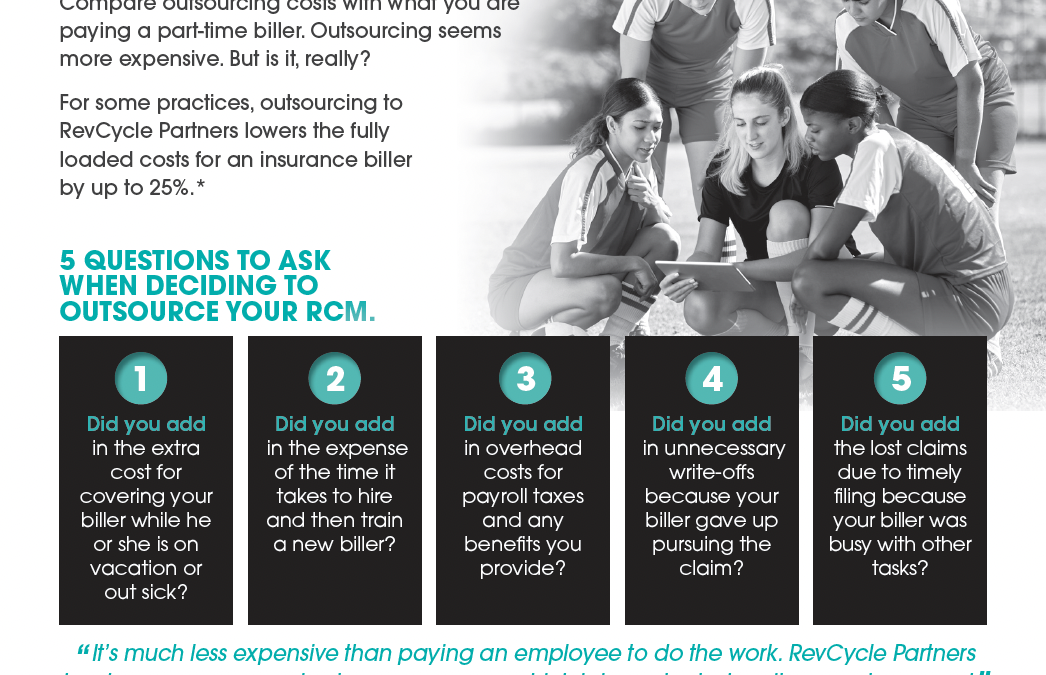
The Hidden Costs of an In-House Biller
Five Hidden Costs of an In-House Biller Outsourcing seems more expensive. But is it really? We've identified the 5 questions you should ask to identify the hidden costs of keeping an in-house biller. You might be surprised by what you find out. Download the PDF »

Testimonial 028
Our credentialing rep was just awesome. Very professional and always on top of our credentialing for our new associate. She made the process very streamlined and super stress free for us as we could trust her to get it done. She checked in regularly and genuinely cared. It was very refreshing to have the experience that we did and can’t say enough how thankful we were to work with her. Dr. Kyler KnobbeVision Source Wamego / Manhattan

Testimonial 027
With RevCycle, deposits come in quickly and efficiently and I don't have to worry about it! Dr. Jennifer KeadyFamily Eyecare of Harney County

Testimonial 026
Our biller is the absolute best, and we love working with her. Hiring RevCycle to handle our billing was one of, if not, the best business decisions I have ever made. Dr. Katarzyna BabinskiLudlow Eyecare

Testimonial 025
RevCycle takes the headache out of the practice when it comes to insurance billing/filling/refilling. They have increased our receipts because of no delays in billing and loss of payment for timely filing. Susan Nelson, Office ManagerSt. Anthony Eye Clinic

Testimonial 024
We love our medical biller, she has taken such great care of us. RevCycle is an awesome partner. Deb JaegerEye Center of the Dakotas

Former RevolutionEHR Co-Founder and CTO Jim Schneider Joins RevCycle Partners
As the new CTO, Schneider will lead the development of the technology infrastructure to support the company’s U.S.-based revenue cycle management team. September 12, 2022 CHICAGO, IL – Former RevolutionEHR Co-Founder and CTO Jim Schneider has joined RevCycle Partners as Chief Technology Officer. As CTO, Schneider will lead the design and build out of a comprehensive RCM Portal to support RevCycle Partners’ rapidly growing team of insurance billers, eligibility and benefits team members, and...

RevCycle Partners Co-Founder and Executive Vice President Recognized as a Most Influential Woman in Optical
Vision Monday celebrates Christine Schneider as a female executive who has shaped the eyecare industry. August 23, 2022 CHICAGO, IL – Vision Monday recently named its 2022 Most Influential Women in Optical, and Christine Schneider, Co-Founder and Executive Vice President of RevCycle Partners, made the list. For twenty years, Vision Monday, the optometry industry's leading source of news and news analysis, has recognized those women who have made a positive difference in the field of optometry....

7 Questions to Ask before You Hire a Freelance Insurance Biller
Beware of the security concerns before you outsource your billing and hire a freelance insurance biller. The Covid 19 crisis reshaped work in America. According to recent polls, one by the Pew Research Center and another by the Becker Friedman Institute for Economics at the University of Chicago, the majority of Americans prefer to work from home—and the majority of workers are at the very least partially working from home. Even though the percentage of work-from-home workers is slightly lower...

Credentialing through a Practice Transition
A Q&A with the RevCycle Partners Credentialing Team Credentialing your optometry practice through a practice transition can feel like jumping through endless hoops. You hop through one, and another pops up. Hoops include opening a new practice, adding a new grad, adding a new doctor, or changing your name because of marriage or divorce. During transitions, it’s critical to pay attention to your credentialing, even though it feels tedious. Recently, a few optometrists asked our...

How WeVerify Works
Manager Cindy Miller Provides an Inside Look

How to Handle Insurance Payer Denials
understanding payer guidelines Brought to you by RevCycle Partners, this webinar presents strategies on how to handle insurance payer denials. Payer customer service representatives are in the business of denial, and they hold most of the power. But you don’t have to accept what the payer says to be correct. The best way to handle insurance payer denials is to have a thorough understanding of payer guidelines, be specific when inquiring about the denial, and ask specifically why the claim is...
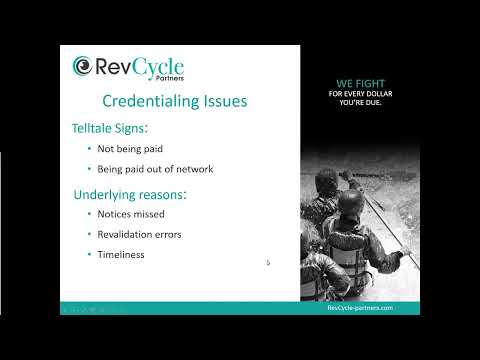
How to Avoid Common Credentialing Issues
most common ways to know if you have a credentialing issue Brought to you by RevCycle Partners, this webinar discusses how to avoid common credentialing issues. The two most common ways to know if you have a credentialing issue are: if you’re not being paid; and/or if you’re being paid out of network. The most common underlying reasons for credentialing issues are notices missed, revalidation errors, and lack of timeliness. One of the most common credentialing issue is the application process....
Testimonial 010
We have multiple locations, which means there are many claims going out the door on a daily basis. RevCycle Partners is efficient and ensures clean billing. Anytime I've had an issue they are quick to resolve it.
Testimonial 009
I use RevCycle for medical billing. I have outsourced to at least 3 or 4 different services over the years. When I started with RevCycle my AR was a mess from the prior biller. They have been amazing in cleaning it up.
Testimonial 008
We use RevCycle and have had great success. They are quick to get claims filed and do a great job working our aging. We have a good relationship with our RevCycle Partners representative. She lets us know if we are leaving off anything, like diagnosis codes, and always answers any questions we may have.
Testimonial 007
We absolutely love our RevCycle Partners representative. She scrubs our claims, finds errors that we would have never caught. She shows us our mistakes, so we can be better informed next time.
Testimonial 006
We use RevCycle for vision and medical billing. It has freed up an entire staff person to focus on patient care. They post everyday so it’s been a lifesaver to keep the A/R down.

Jon Kettner
IT & Security Responsible for IT and Security, Jon plays a behind-the-scenes role that keeps RevCycle Partners operating smoothly. Jon manages all aspects of our IT infrastructure, including endpoint PC deployment, helpdesk, and administration of our cloud applications. Given our health care domain, Jon gives priority to all things security related. He defines and monitors our security policies, security training, and HIPAA compliance policies. Jon has a broad background in both RCM and...

Casey Squicquero
Staff Development Casey is responsible for staff development at RevCycle Partners. This includes the onboarding of new hires as well as supporting the existing employees with ongoing training. Casey manages the creation and delivery of training content and the RevCycle Partners’ knowledge base. This role puts her in a unique position to provide evaluation of the RevCycle staff to ensure quality and consistency of the delivery of our services. Like many of the billers at RevCycle Partners,...

Sarah Ester
Sales Sarah is responsible for the sales of all RevCycle Partners’ services - billing, credentialing, and verification. She works directly with eyecare practices that are vetting RevCycle Partners as an outsourcing partner and is chartered with assisting them to determine if RevCycle is a good fit for their practice. Sarah was naturally drawn to the optometry space as her father is an optometrist. She first worked for him as an optometric technician and later assisted the practice when they...

Dave Kegel
WeCredential Dave manages the credentialing team along with the 100s of credentialing projects performed by RevCycle each year. He is an experienced technical and project manager with expertise in building teams and creating processes, skills he brings to his leadership of the WeCredential service. Dave has significant start-up experience, having helped build multiple firms from early-stage startups through acquisition by large technology or private equity firms. Dave was introduced to the...

Cindy Miller
WeVerify Cindy manages the WeVerify team at RevCycle Partners, delivering eligibility and benefits verification services to our customers. She fronted the launch of this service and built the team from scratch. With 30+ years in healthcare administration, Cindy is uniquely qualified to lead the WeVerify team at RevCycle Partners. Cindy brings management experience from running practices in various health care verticals, including emergent care, internal medicine, and OB-GYN. She was introduced...

Amanda Kissinger
Software Platform Expansion After the launch of RevCycle Partners as an independent RCM company, Amanda took on the responsibility of expanding RevCycle Partners’ support of the leading optometric EHR/PMS software. A critical component to RevCycle Partners’ growth, she now leads a team of managers and billers servicing practices on these platforms. Amanda brings over ten years of eyecare billing experience to RevCycle Partners. She lucked into the optometry space in college while looking for a...

Dave Wright
Finance & Accounting Dave fronts the finance and accounting areas for RevCycle Partners and is responsible for financial systems, financial reporting, and our banking relationships. Dave brings in-depth knowledge and experience to RevCycle Partners, having spent 30+ years managing finance & HR operations at startups, Fortune 500, and Big 4 accounting firms. Dave also brings back-office experience from a breadth of eyecare enterprises. He has provided financial and accounting services...

Dave Goetz
Marketing With over twenty years in strategic marketing, working with more than 250 companies in health care, technology and financial services, Dave oversees the marketing strategy and the implementation of marketing programs for RevCycle Partners, including development of branding, messaging, marketing campaigns, and coordinating efforts with the company’s sales goals. Dave got his start in the optometric industry through an engagement with RevolutionEHR. He was responsible for the...

Jim Schneider
Technology Development With a long history of developing web-based systems in healthcare IT, Jim Schneider joined the RevCycle Partners team in 2021 to lead the development of our internal technology systems. The focus of Jim’s team is the development and deployment of the RevCycle Operations Center. This platform provides workflow automation for all aspects of the RevCycle Partners’ business, including management reporting and auditing, customer onboarding, and daily staff workflow. Jim has...

Melissa Jacobson
RevCycle Operations In her role as Operations Manager, Melissa works with RevCycle Partners’ team of managers and billers to ensure a consistently superior billing service. Melissa also takes seriously her role mentoring insurance billers, developing staff, and managing resources. Melissa fell in love with optometric patient care when she stumbled into a technician role at a local practice. Serving 12 years at a ten-location practice with a mixture of LensCrafters subleases and Pearle Vision...

Christine Schneider
Executive VP of Services & Co-Founder Christine co-founded RevCycle Partners and is the Executive VP of Services for the company. In this role, she oversees the service delivery for all RevCycle Partners’ lines of business, including the development and roll-out of new service offerings. Christine’s career spans 25 years of billing experience beginning in chiropractic and laboratory pathology settings prior to transitioning to eyecare. As is often the case in a private practice setting,...

Paul Hartge
CEO & Co-Founder Paul, the CEO and co-founder of RevCycle Partners, is responsible for the strategic direction, operational success, and financial health of the business. He oversees strategic partnerships and industry relations as well as manages the board and investor relations. In 2008, Paul entered the optometry space as COO of RevolutionEHR. A longtime entrepreneurial software executive who has successfully built and sold technology start-ups, Paul spearheaded the growth of...

Testimonial 023
We have multiple locations, which means there are many claims going out the door on a daily basis. RevCycle Partners is efficient and ensures clean billing. Anytime I've had an issue they are quick to resolve it. We love it! Melissa HaightHarrel Eyecare

Testimonial 022
WeVerify will be like Recall. Every practice will need it. Dr. BrandonWeVerify User

Testimonial 021
RevCycle has been great to work with for our billing, credentialing, and eligibility verification. They made my job so much easier over the years. Sarah TurnerPrimary EyeCare Centers

Testimonial 020
The best move I’ve made in 21 years of business was to outsource to RevCycle. It would have saved so many cashflow dips if I’d partnered with them the first 12 years. Dr. Monte HarrelHarrel Eyecare

Testimonial 019
I have been pleased with the years of both billing and credentialing services and will continue to recommend RevCycle Partners. Dr. Laurence LonkyCortlandt Eye Care

Testimonial 018
Thank you for all that you do to keep our accounts - our insurance A/R has never been lower! Heidi HipsherNorthland Eyecare

Testimonial 017
Our RevCycle biller is very professional, accurate, fast and is like a terrier getting every claim processed to the maximum benefit. We are happy to have her as part of our team. Paul LatkaChicopee Eyecare

Testimonial 016
Best decision we ever made. It’s not cheap but it’s consistent and saves you headaches of hiring, training, benefits, etc. Dr. Makenzie ElliottElliott Eye Doctors

Testimonial 015
We use RevCycle and like it! It’s much less expensive than paying an employee to do the work. They have been very responsive to any concerns which is important when it comes to money! Dr. Angela BerghoffLoman Eye Care

Testimonial 014
We use RevCycle and have a fabulous specialist assigned to us. We use them for posting of medical claims and working the A/R. Elaine StewartWhidbey Vision Care

Testimonial 013
I use RevCycle for both medical and vision billing. I learned the hard way and I’ll pay for the peace of mind that my claims are being submitted, and submitted properly and timely. Dr. Jason KaminskiVision Source Longmont

Testimonial 012
We appreciate the tremendous efforts and payouts by your billing staff. I don’t foresee us wanting to take medical billing back in house any time soon. It has lifted a load! Talli Vance, Practice AdministratorVance Vision Clinic

Testimonial 011
Thanks a million times for your compassionate handling of your customers through the COVID pandemic. RevCycle billing services just about saved my life in February-March and the WeVerify service has proven extremely useful. Jen Heller, Business ManagerPend Oreille Vision Care

Testimonial 010
I use RevCycle for medical billing. I have outsourced to at least 3 or 4 different services over the years. When I started with RevCycle my AR was a mess from the prior biller. They have been amazing in cleaning it up. Dr. Sarah Paikowsky

Testimonial 009
Our previous biller retired so we decided to outsource our billing to RevCycle and couldn’t be more pleased. Our transition was very smooth and we have not experienced any problems. We appreciate the outstanding service provided by RevCycle. Lori Dobson, Office ManagerVision Source Mustang

Testimonial 008
RevCycle has been a valuable partner to our practice. Dr. Scott BraseIsland Family Optical

Testimonial 007
We use RevCycle for vision and medical billing. It has freed up an entire staff person to focus on patient care. They post everyday so it’s been a lifesaver to keep the A/R down. Dr. Natalie SukontasupFirst Sight Vision Care

Testimonial 006
We have multiple locations, which means there are many claims going out the door on a daily basis. RevCycle Partners is efficient and ensures clean billing. Anytime I've had an issue they are quick to resolve it. We love it! Melissa HaightHarrel Eyecare

Testimonial 005
We use RevCycle and have had great success. They are quick to get claims filed and do a great job working our aging. We have a good relationship with our RevCycle Partners representative. She lets us know if we are leaving off anything, like diagnosis codes, and always answers any questions we may have. Jennifer Carter, OptometristWest Georgia Eye Care

Testimonial 004
We absolutely love our RevCycle Partners representative. She scrubs our claims, finds errors that we would have never caught. She shows us our mistakes, so we can be better informed next time. Jolean DresbachSanderson Eye Clinic

Testimonial 003
We could not be happier with RevCycle Partners. Our biller doesn't miss a thing. We were leary after a horrible experience with another billing company, but we are thrilled with RevCycle Partners! Katy Baldry, Office ManagerSanderson Eye Clinic

Testimonial 002
My main billing person loves RevCycle Partners. Our AR is under good control. They are less expensive than another billing employee. David Wolf, OptometristLake Oswego Vision Clinic

Testimonial 001
It’s been a real lifesaver using RevCycle Partners the past few years. Your crew has done a terrific job, and I have recommended your services to anyone who has asked (and several who have not!). Kelly has been great to work with and very patient. Jean Wrightnour, O.D.

Time to Revalidate Your Medicare Enrollment!
It’s time to revalidate your Medicare enrollment By Dave Kegel, Manager of Credentialing Two years ago, during the COVID-19 Public Health Emergency (PHE), Centers for Medicare & Medicaid Services (CMS) enacted a waiver that allowed new, non-certified Part B suppliers, physicians, and non-physician practitioners to obtain temporary Medicare billing privileges. CMS also temporarily waived the associated application fee, criminal background checks, and site visit requirements. All Medicare...

What to Do When You Face Insurance Payer Denials
When insurance payer denials continue to wreak havoc By Amanda Kissinger, RevCycle Partners Billing Service Group Manager The best insurance billers are tenacious. They have to be. And yet insurance payer denials continue to wreak havoc. Think of the number of times an insurance payer denies payment. You did your research. You used the right CPT codes for the service provided. You reported the necessary additional information, such as the referring provider. You know it was posted within the...

3 Reasons Optometry Practices Outsource
Reasons Optometry Practices Outsource By Melissa Jacobson, Operations Manager While there are many reasons optometry practices outsource, it’s never an easy subject to discuss with staff. When the subject of outsourcing comes up, the office mood can tighten. Staff can feel threated as they wonder, Will my role be eliminated? Am I not doing a good enough job? In some cases, the job simply isn’t getting done, and outsourcing every aspect of the function is a necessity for practice survival. High...

Commonly Misused Coding Modifiers
MODIFIERS ARE COMPLICATED By Melissa Jacobson, Operations Manager Using the incorrect procedure modifiers—or missing them altogether—can lead to denials. Denials, of course, mean delays in payment, or worse, non-payment. As a refresher, below are commonly misused coding modifiers for optometry insurance billing. MODIFIER 25:“Used for significant, separately identifiable evaluation and management service by the same physician on the same day of the procedure or other service.” This is most...

How Eligibility and Benefits Verification Create A Better Patient Experience
“BUT PATIENTS WILL BE ANNOYED! THEY DON’T WANT TO BE BOTHERED.” By Christine Schneider, VP of Operations That’s what many patient care coordinators may think when faced with the decision of whether to verify eligibility and benefits by phone prior to a patient’s visit. But what if that extra step actually creates a better patient experience? What if the call makes the patient happier in the long run? Eligibility and benefits verification is advantageous to patients. Practices can collect the...

Alleviate Your Transition Period: Outsource Your Insurance Billing
IS YOUR OPTOMETRY PRACTICE IN TRANSITION? By Amanda Kissinger, Billing Services Group Manager Maybe you’re growing and buying up a practice or two. Or maybe your practice is being purchased. Or maybe because of the pandemic-induced staffing shortages, you’re having trouble hiring staff. Whatever the reason for the transition, it likely will be a chaotic time for your practice. If you outsource your insurance billing, even for a brief period, you can alleviate some of your stress. If you’re...

Medicare Denials for Glasses after Cataract Surgery
MEDICARE DENIALS By Amanda Kissinger, Billing Services Group Manager Medicare denials are perplexing. And frustrating. One small detail missed—and a service won’t be covered. Particularly frustrating are Medicare denials for glasses after cataract surgery—even though you are credentialed with Medicare. What’s going on? Here Are Some Helpful Tips To Keep In Mind To Ensure You Don’t Have To Deal With Medicare Denials For Glasses: Glasses after cataract surgery are considered medically necessary...

Improve Your AR with Electronic Payments
MAIL DELIVERY IS SLUGGISH Blame it on the Covid pandemic or the politicization of the system, but the United States Postal Service’s delivery rate bottomed out at 62 percent—the lowest in years. It rebounded a bit by March of 2021 to 84%. But even that number falls short of the agency’s target of 96%. If your optometry practice receives a bulk of its payments or processes claims by snail mail, your AR could suffer. You can improve your AR with electronic payments. When you process claims...

The Hidden Complexities of Credentialing a New Doctor
credentialing a new doctor By Christine Schneider, VP of Operations Credentialing Seems Simple But even practices that pride themselves in being on top of credentialing can find themselves floundering with one small oversight. One area practices often get tangled up in is credentialing a new doctor who recently graduated. Take, for example, an established community optometry practice in Kansas that signed on a new associate—a recent optometry grad. Since the doctor was a new grad, the office...

Details on the 2021 ABN Update
ABN Update By Melissa Jacobson, Director of Insurance Billing In January 2021, the Centers for Medicare and Medicaid Services (CMS) revised the Advanced Beneficiary Notice of Non-coverage (ABN) Form. The ABN Form CMS-R-131 is issued to the patient or client by providers, physicians, practitioners, and suppliers in situations where Medicare payment is expected to be denied. The biggest change to the ABN is the special guidance that was added for people who are dually enrolled in both Medicare...

New Evaluation and Optometry Coding Changes for 2021
Optometry coding changes By Casey Squicquero, Billing Support Group Manager, RevCycle Partners The new year always brings new coding guidelines. Here are a few coding changes for 2021. Rather than using history, examination, medical decision-making and time to determine the level of E/M service, like providers have always used, the update to the E/M coding guidelines will be determined based on 1 of 2 factors: 1. Level of service is defined by medical decision-making for the service. Medical...

6 Vexing Insurance Billing Questions for Eyecare Practices
common insurance billing questions that stump the best of us By Christine Schneider, VP of Operations If you’re an insurance biller for an optometry practice, you’re a master problem solver. Each patient is unique, their needs and their coverage. But even the most experienced billers run into vexing billing questions. Here are a few common insurance billing questions that stump the best of us — and their answers to help you provide better optometric patient care. Insurance Billing Question...
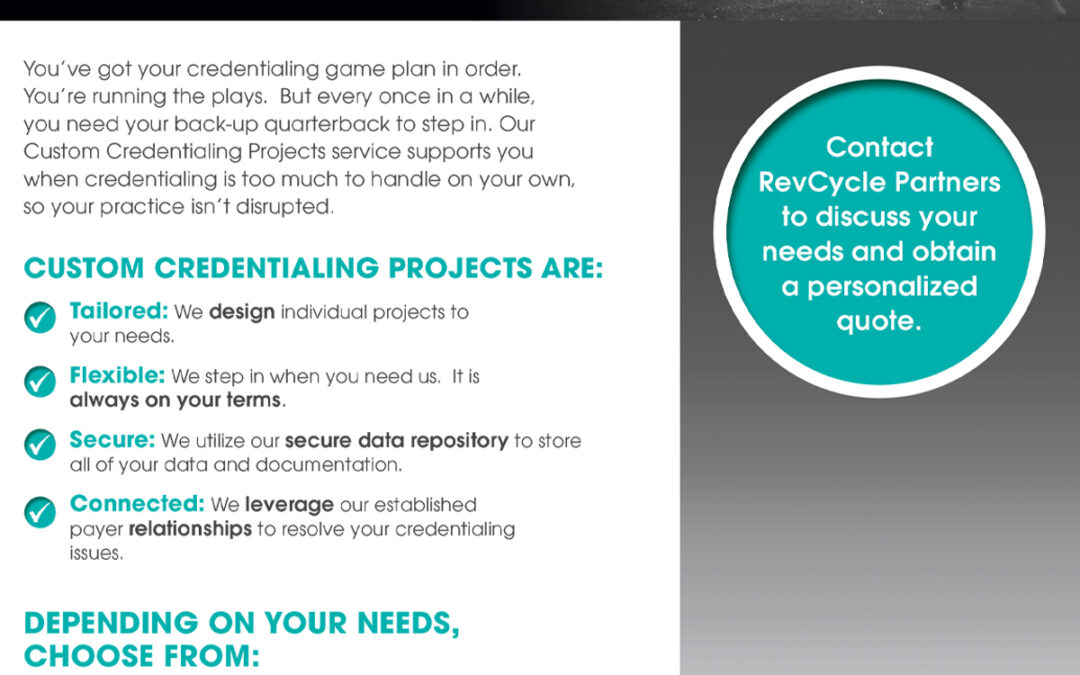
WeCredential Custom Credentialing Projects
Tailored solutions for your practice. You’ve got your credentialing game plan in order. You’re running the plays. But every once in a while, you need your back-up quarterback to step in. Our Custom Credentialing Projects service supports you when credentialing is too much to handle on your own, so your practice isn’t disrupted. Download the PDF »
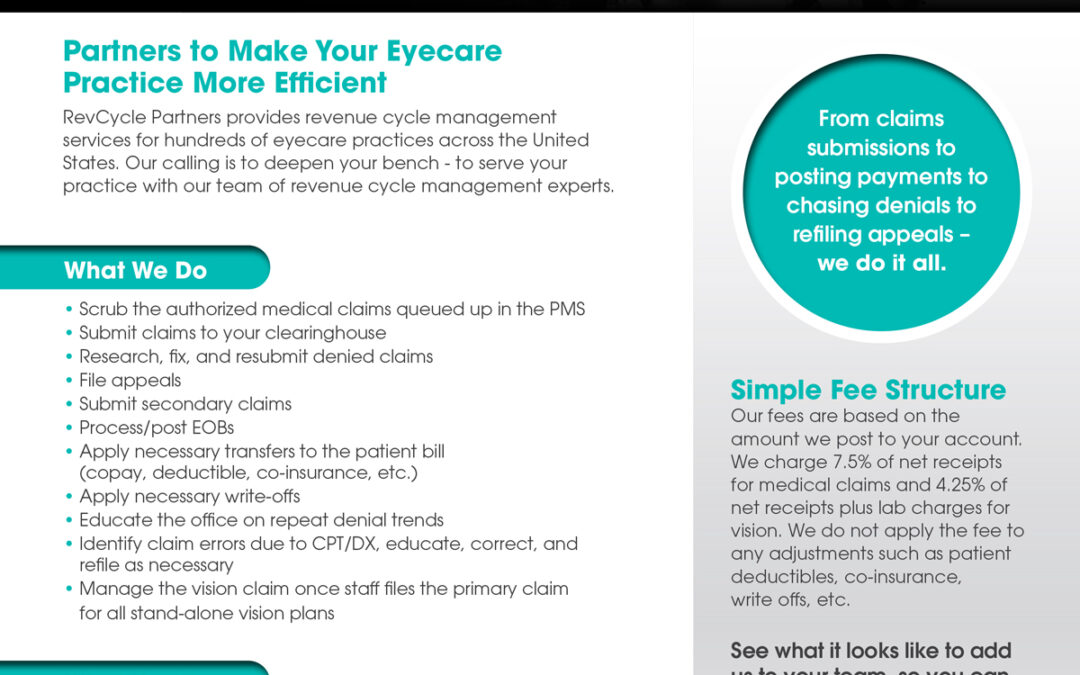
Your Bench Just Got Deeper
Revenue Cycle Solutions for the Eyecare Industry RevCycle Partners provides revenue cycle management services for hundreds of eye care practices across the United States. Our calling is to deepen your bench - to serve your practice with our team of revenue cycle management experts. Download the PDF »
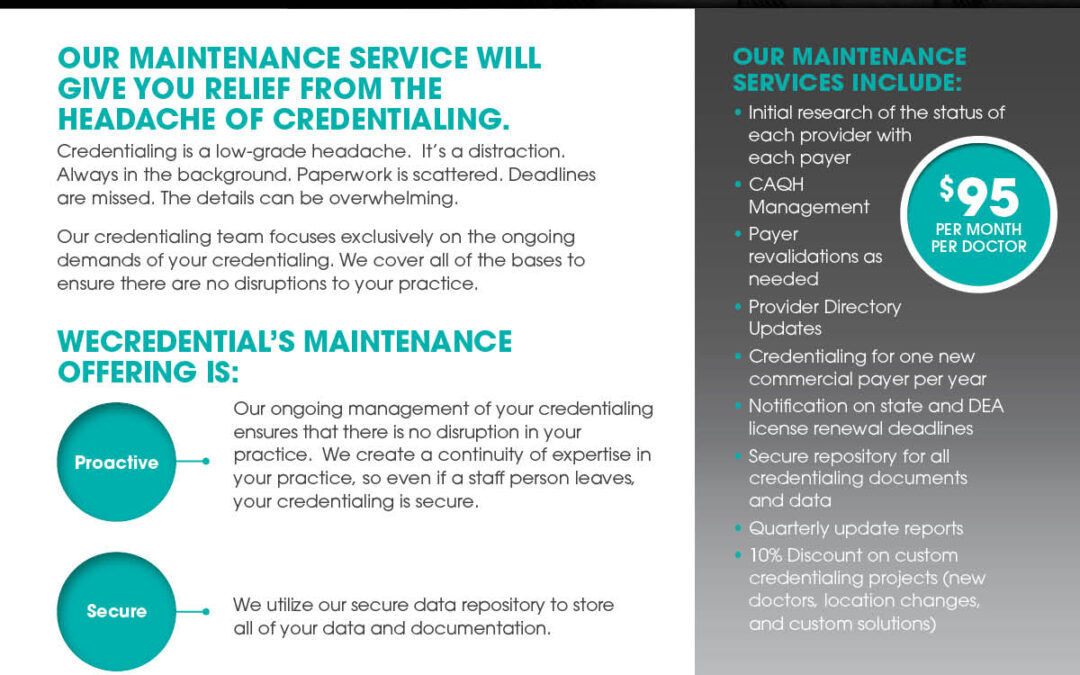
WeCredential Maintenance
A proactive approach to staying on top of your credentialing. Credentialing is a low-grade headache. It’s a distraction. Always in the background. Paperwork is scattered. Deadlines are missed. The details can be overwhelming. Our credentialing team focuses exclusively on the ongoing demands of your credentialing. We cover all the bases to ensure there are no disruptions to your practice. Download the PDF »
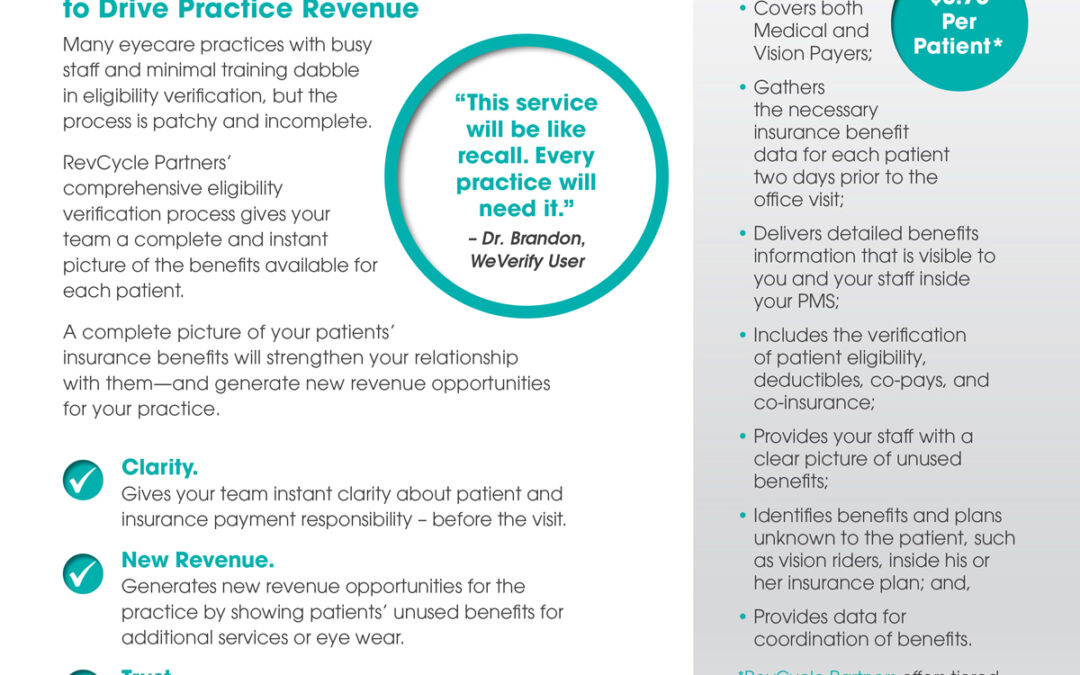
WeVerify
Confirm Patient Benefits Many eyecare practices with busy staff and minimal training dabble in eligibility verification, but the process is patchy and incomplete. RevCycle Partners’ comprehensive eligibility verification process gives your team a complete and instant picture of the benefits available for each patient. Download the PDF »

Why Should You Outsource Your Credentialing?
OUTSOURCE YOUR CREDENTIALING. Brought to you by Professional Eye Care Associates of America (PECAA), and in partnership with RevCycle Partners, this webinar discusses problems related to credentialing and why you should outsource your credentialing. Listen to the stories of optometrists about the difficulties with credentialing in-house, how credentialing problems can sideline your practice, and the benefits you reap when you outsource your credentialing. In this webinar, RevCycle Partners...
How to Avoid Claim Denials: Underlying Issues with Credentialing
AVOID CLAIM DENIALS. Brought to you by RevCycle Partners, this webinar explains how you can avoid claim denials by addressing the underlying issues with credentialing. Learn more about four issues that lead to claim denials: complicated application process, confusion around closed networks, lack of tracking and documenting, and not understanding your state Medicaid process. These issues tend to be the leading causes of denials, and make it more difficult to avoid claim denials. As part of this...

How to Improve Your Eligibility and Benefits Verification Process
IMPROVE YOUR ELIGIBILITY AND Benefits VERIFICATION PROCESS. Brought to you by RevCycle Partners, and in partnership with RevolutionEHR, this webinar discusses how you can improve your eligibility and benefits verification process for a smoother patient experience. Learn more about the difficulties in the verification process, what questions the verification process answers, and how verification data can drive revenue. If you want to improve your eligibility and benefits verification process,...
How to Simplify Billing for Medicare and Medicaid
BILLING FOR MEDICARE AND MEDICAID. Brought to you by RevCycle Partners, this webinar discusses the struggles of billing for Medicare and Medicaid and provides tips on how to simplify billing. It is difficult to navigate Medicare and Medicaid, from billing wrong payers to receiving denials for medical necessities. The simplest tip when billing for Medicare and Medicaid: you need to have a firm understanding of what your practice is credentialed for and the plans and coverage you accept when it...
How to Successfully Bill Insurance
SUCCESSFULLY BILL INSURANCE. Brought to you by RevCycle Partners, and in partnership with RevolutionEHR, this webinar presents various tips on how to successfully bill insurance. The best way to successfully bill insurance is by collecting the necessary information up front. By collecting insurance information as soon as possible, you can explain to the patient which of their plans are active and what benefits they qualify for, which sets you up for a smooth billing process. And when you use...

How to Work Your Aging Claims
WORK YOUR AGING CLAIMS. Brought to you by RevCycle Partners, and in partnership with RevolutionEHR, this webinar explains how your practice can stay on track of aging claims, and how you can work your aging claims. Learn useful tips on how to prevent aging claims from occurring and how to work your aging claims once they appear. In this webinar, you will, more specifically, learn about processes and procedures surrounding AR. To prevent aged claims from occurring, you should periodically...

Why You Should Outsource Your Eligibility and Benefits Verification
OUTSOURCE YOUR ELIGIBILITY AND BENEFITS VERIFICATION. Brought to you by RevCycle Partners, and in partnership with RevolutionEHR, this webinar explains why you should outsource your eligibility and benefits verification. When compared to outsourcing insurance billing, outsourcing E&B verification is not as common, yet E&B verification is important for a smoother patient experience. Learn more about implementing a robust verification process, the problems associated with verification...

Why Should You Outsource Your Insurance Billing?
OUTSOURCE YOUR INSURANCE BILLING. Brought to you by RevCycle Partners, this webinar discusses whether you should outsource your insurance billing. A group of panelists tackles various questions that concern outsourcing. Learn more about the value of outsourcing when you’re understaffed or in transition, what specifically your eyecare practice should outsource, and how you can strategically and effectively outsource your insurance billing. In this webinar, you will learn what outsourcing is and...

Options to Outsource Your Insurance Billing
OUTSOURCE YOUR INSURANCE BILLING. Brought to you by RevCycle Partners, and in partnership with RevolutionEHR, this webinar provides an overview of what it looks like to outsource your insurance billing. Learn more about the outsourcing options for your practice and how outsourcing can help when you’re wrestling with staffing issues. This webinar also provides a general overview of outsourcing and tackles common misconceptions practices have when it comes to outsourcing their insurance billing....

Why You Need to Prioritize Eligibility and Benefits Verification
PRIORITIZE ELIGIBILITY AND BENEFITS VERIFICATION. Brought to you by RevCycle Partners, and in partnership with RevolutionEHR, this webinar explains why your practice should prioritize eligibility and benefits verification. Learn more about the hidden costs of an E&B verification system, why implementing an E&B verification system can be tedious, where practices can struggle when trying to verify E&B, and why a practice should consider outsourcing. In this webinar, RevCycle Partners...

How to Tackle Eligibility and Benefits Verification in Your Practice
ELIGIBILITY AND BENEFITS VERIFICATION IN YOUR PRACTICE. Brought to you by RevCycle Partners, this webinar presents strategies you can employ when you tackle eligibility and benefits verification in your practice. Determine your practice’s commitment level to E&B verification and learn more about the key returns of E&B investment. When you tackle eligibility and benefits verification in your practice, there will be less downstream billing mistakes, more revenue opportunities, and a...
Embracing Outsourcing as a Strategy
IS IT TIME TO RETHINK YOUR STRATEGY When it comes to outsourcing your optometry office’s functions, it’s natural to look only at the direct costs. You analyze your in-house staff wages. And then compare them to a vendor’s fees. But there’s more to it than a basic wage to fee comparison. And it’s not an all-or-none decision. Here are some reasons for embracing outsourcing as a strategy. Free to Focus on Your Care Outsourcing at its best augments a practice’s team, with the outsourcing vendor...

Advances in Improving Aging Claims Process
HOW REVCYCLE PARTNERS IS CHANGING AND IMPROVING THEIR AGING CLAIMS PROCESS. By Melissa Jacobson, Operations Manager of RevCycle Partners Transparency translates to accountability. And accountability translates to better service. That is why we are improving our aging claims process. Our goal, each month, is to touch every aging claim, and place them in front of you in an easily digestible format. At the beginning of each month, you will receive a spreadsheet of all aging that is 46 days and...

How to Account for a Medicare Pre-Payment
DO YOU HAVE QUESTIONS ABOUT HOW TO ACCOUNT FOR A MEDICARE PRE-PAYMENT? By Christine Schneider, Vice President Do you have questions about how to account for a Medicare pre-payment? Read below for some helpful tips. Create a Medicare Invoice The best way to account for a Medicare pre-payment in RevolutionEHR is to create a Medicare invoice (inside of a dummy patient) and apply that payment to the invoice to generate an invoice credit. Process EOB as Normal, But Apply Same Total as a Negative...

Update on Medicare Reimbursements for Telemedicine Visits
WHAT YOU NEED TO KNOW ABOUT THE RECENT CHANGES. By Christine Schneider, Vice President In these unprecedented and difficult times, we want to help you as you navigate the changes on Medicare reimbursements for telemedicine visits. Click on the link below for the latest in Medicare’s reimbursement for telemedicine visits while we are faced with national emergency due to Covid-19. The Trump Administration just announced expanded Medicare telemedicine (non-face to face visits) coverage that will...
Avoid Billing Detours for Co-Managing Cataract Care
THREE THINGS TO KEEP IN MIND TO EASE CO-MANAGING CATARACT CARE. By Melissa Jacobson, Operations Manager Co-managing cataract care with ophthalmologists is one way you can provide continuity of care to patients before and after surgery. But the logistics of transfer of care can be tricky, and, if not addressed correctly, can slow down the billing process. Here are three things to keep in mind to ease co-managing cataract care: 1. Completely and accurately fill out the patient consent form. All...

2 ODs Share Their Struggles with Eligibility and Benefits Verification
WHY YOU NEED A SYSTEM TO IMPROVE AR AND PATIENT CARE. Gather a group of optometrists to talk about the challenges of operating an eyecare practice, and their struggles with eligibility benefits verification will likely crop up. Docs know they should be doing it, but it often is incomplete or sporadic. RevCycle Partners recently chatted with two seasoned eyecare practitioners, Dr. Jennifer Carter of West Georgia Eye Care and Dr. Carolyn Martin of Eye Boutique of Sedona, about implementing a...

Growing Pains of a Growing Practice: The Benefits of Outsourcing Your Credentialing
A CASE STUDY ABOUT THE BENEFITS OF OUTSOURCING YOUR CREDENTIALING. By Jon Kettner The Growing Pains of a Growing Practice: A large optometry practice—with multiple locations, more than 20 providers, and spanning two states—was growing faster than its half-day credentialing specialist could keep up with. Without a dedicated full-time staff, revenue cycle management issues cascaded. The leaders of the practice worried about cash flow implications and how to credential their docs more quickly. It...

Changes to Medicare in 2020
WHAT YOU NEED TO KNOW ABOUT MEMBER IDS, DEDUCTIBLES, AND MEDIGAP PLANS. By Christine Schneider Billing Medicare can be dizzying work because of the multiple updates to policies from year to year, and sometimes even from month to month. In 2020, there are changes to Medicare that will affect your billing if not handled correctly. Below are three changes to make note of now, so you hit your stride on January 1st. Changes to Medicare Member IDs on January 1 You must submit claims with the...

Important Changes to Credentialing for 2020
MAKE NOTE OF THESE IMPORTANT CHANGES TO CREDENTIALING FOR 2020. By Jon Kettner For many optometry practices, the new year is a time when practices ask, “What are my growth goals?” Growth, of course, is tied to healthy revenue cycle management. The new year is the perfect opportunity to make sure you’re aware of changes to credentialing in your state. Below are some changes to credentialing to make note of for the new year. If you want to add another insurance, the average insurance turnaround...

Coordinating Benefits for Your Eyecare Practice – 3 Easy Steps
A START-TO-FINISH PROCESS. By Christine Schneider, VP of RevCycle Partners Coordinating benefits for your eyecare practice is complicated. Optometrists have to deal with coordinating medical and VSP benefits. Here are a few guidelines for coordinating benefits for your eyecare practice — to streamline billing, increase cash flow, and better serve patients: Know What’s Primary, What’s Secondary A patient with multiple medical insurance plans always has a primary payer and secondary payer. A...

Billing Medicare and Medicaid
A START-TO-FINISH PROCESS. By Christine Schneider, VP of RevCycle Partners Billing Medicare and Medicaid can be a messy process. If not handled correctly, it can affect payment and even patients—who might be billed more than expected. There are multiple pain points that begin the moment the appointment is made and end with payment collection. Here are 7 Tips to simplify billing Medicare and Medicaid from start to finish: Stay on Top of Your Credentialing. You might be sick of hearing it, but...

Outsourcing to Improve the Cash Flow of Your Practice
QUESTIONS TO ASK TO DETERMINE IF IT WILL BENEFIT YOUR EYECARE PRACTICE. In “The Review of Optometric Business,” Peter J. Cass, OD claims that you could improve the cash flow of your practice by outsourcing your billing. But will it really? In “Improve Cash Flow by Outsourcing Billing and Coding”, Coss offers a series of questions to help you determine whether outsourcing will really help to improve the cash flow at your eyecare practice. Questions include: How long do claims sit in your...

Want a More Efficient Eyecare Practice?
TIPS TO CUT TIME SPENT ON ADMINISTRATIVE WORK AND INSURANCE OBSTACLES. Staying on top of administrative tasks and insurance billing is key to making a more efficient eyecare practice. And that means you’ll likely be more profitable. There are a bundle of tasks to do so your practice stays on top of the rapidly changing healthcare system. When you’re on top of the administrative tasks, your patients actually reap the benefits. In a recent article, “5 Ways to Make Your Practice More Efficient”...

Do You Have Time to Be Present with Your Patients?
AN ESSAYIST DISCUSSES THE CHALLENGE OF MAKING MORE TIME FOR FACE-TO-FACE INTERACTION IN A TECH ERA. Staying on top of your optometry practice’s details–whether filling out electronic records or tending to details related to insurance billing and credentialing–has a way of making you feel like you don’t have time to be present with your patients. In the article “Be Present with Your Patients,” an essayist discusses how technology has caused many doctors to compromise the very thing they went...
Is there a set-up fee?
No.
What is the contract length?
There is no long-term commitment. You may cancel at any time. We ask for a 60-day termination notice so we can properly wind down the account and reallocate our resources.
Do you obtain benefits for same-day appointments or walk-ins?
We do not. We guarantee the schedule two days ahead of the visit. Any new appointment that falls within that 48-hour window would be the office’s responsibility.
Do you obtain benefits for out-of-network insurances?
While we can and do obtain benefits for out-of-network Medical plans, we are not able to obtain benefits for out-of-network Vision plans. On the Vision side, it is becoming harder to obtain benefits for OON payers. Many payers, like VSP, are directing users to have their patients contact the payer directly or send claims in for out-of-network services.
Will remaining deductible amounts be verified?
Yes, WeVerify will obtain the deductible and remaining deductible amounts.
How do you ensure the accuracy of what a patient owes towards his/her deductible?
The deductible is tallied based on who gets to the insurance first and applied in that order. We are given information based on the date and time asked. Things can be processed after and in-between. Offices that know their fee schedules can collect most accurately.
Do you pull authorizations for VSP? What about medical documents?
Yes, WeVerify will obtain authorizations from Vision Plans and upload them into the PMS for office use. WeVerify does not upload Medical documents into the PMS.
Can we choose which patients you verify, or can we pick which insurances are verified?
The service was built to provide all benefits for all of a patient’s plans. We feel the value of our service is allowing you the opportunity to utilize the benefits to the fullest. That said, if you have specific needs or concerns, we can schedule a conversation to determine whether a custom design would be favorable.
Does WeVerify obtain medical referrals?
We do not obtain Medical referrals. If a Medical referral is required, WeVerify would notify the office that one is needed, and the office is responsible for obtaining it.
Would WeVerify check benefits for a cataract post-op?
We do not check benefits for cataract post-ops. We do not check benefits for any post-op appointments because generally these appointments are following a recent exam and/or referral where the initial benefits are still valid.
Does WeVerify look for insurance benefits if no insurance is listed for the patient?
If there is no insurance listed for the patient on the schedule, WeVerify will look for any family links for the patient to see if there is an insurance we can try to verify for Medical. For Vision payers, WeVerify will attempt to search for plan benefits by using the patient name and DOB.
Are we charged for verifications that fail because of missing information?
Yes. If WeVerify attempts a verification and is unsuccessful in obtaining information, we will charge for the verification because we took the time and resources to try and verify the benefits.
Does WeVerify write back into my EMR software?
Yes. WeVerify will store the benefit details we obtain in standard templates inside of the practice management system.
Do you require a long- term contract for your maintenance services offering?
Yes. RevCycle Partners requires a two-year agreement for its ongoing credentialing offering called "Maintenance Services." The amount of maintenance work required each month can vary dramatically. Spreading the work and cost out over a 2-year contract creates balance for the practice and RevCycle Partners.
What payers do you monitor under your maintenance service?
Payers that require contracting/credentialing are the ones that would be monitored under the Maintenance Service. Many practices also receive payments from life insurance, Medicare Advantage plans, or Third Party Administrators (TPAs), but those do not require contracting/credentialing. Credentialing with the Advantage Plans is included with the main payer, and revalidations would cover the Advantage Plans for the payer.
Can RevCycle Partners advise on which networks are currently open or closed?
Unfortunately, RevCycle Partners cannot advise on which networks are open or closed. Networks can open and close at any time throughout the year. Networks can also be closed in small, very targeted areas. In many cases, the payer won’t indicate that a panel would be closed for a provider unless an application is submitted. In addition, a network may be closed for one provider and not another in the same area.
What is the difference between in and out of network?
In network means the health care provider has contracted with an insurance plan and approved services are paid according to the contracted fee schedule. Out of network means the health care provider is not contracted with an insurance plan, and benefits will generally process under out of network benefits. This usually means higher out of pocket expenses for the patient.
What is CAQH and do I have to use it?
It is the Council for Affordable Quality Healthcare. Yes, you must have a CAQH profile on file. A majority of the insurance companies use CAQH to confirm information that has been provided to them.
Why do you need my CAQH and PECOS information?
RevCycle Partners will verify and update information as required throughout the credentialing process. Having CAQH and PECOS access reduces paperwork and ensures timely receipt of information.
What happens if the networks are closed and/or request for participation is denied?
Depending on the reason for denial, RevCycle Partners will submit an appeal and/or request participation a second time, 3-6 months later.
Will I be charged if my application is denied?
Yes. RevCycle Partners has verified your information and completed and filed the necessary paperwork on your behalf. We cannot guarantee acceptance. That is solely up to the insurance company to determine.
Once I am credentialed, am I in network for that insurance?
No. For many insurances, being credentialed means you can see patients, but it will pay as out of network.
What is the difference between credentialing and contracted?
Credentialing is the process of establishing the qualifications of licensed medical professionals and assessing their background and legitimacy. Credentialing is required for most insurance companies to be contracted. Contracted means you are an in-network provider and have a signed agreement to accept patients for an agreed fee for service.
Does RevCycle Partners negotiate the fee schedule for me or provide me with a copy of it?
No. All contract negotiations and fee decisions are the responsibility of the practice.
How often will I get an update from you regarding status of my applications?
RevCycle Partners will update information as it’s received from the insurance companies. You can login to your portal account to access any updates noted at any time. RevCycle Partners will provide updates at least once a month.
What happens if the insurance sends me something or reaches out to me directly?
If the insurance reaches out to you or sends you any documentation, it is imperative that you notify a credentialing team member immediately. Failure to forward information from the insurance causes delays. It can also mean having to start the application process over.
How long will credentialing take?
The timeframe all depends on the payer. Some will complete applications in 30 to 60 days. Generally, you should expect the process to take up to 120 days, sometimes longer. We experienced significant delays on payer responses during Covid, and many payers have not caught up yet. Contracting can take an additional 60 days. There are variations in time depending on insurance and reasoning, it can mean shorter and/or longer time frames.
What if I have a part-time doctor?
All doctors expecting to receive reassignment of benefits as a participating provider for claims, must be contracted with the insurance plan, and therefore require credentialing. The amount of time or hours the provider works is not applicable to this requirement.
What if I am already credentialed at another location I work at?
If you are joining a practice within the same state, and you are already participating with payers, demographic updates will take care of linking you to your new practice.If you are joining a practice in a different state, full applications will apply.If you are purchasing or opening a new practice and are establishing a new NPI/Tax ID/company name, brand new credentialing will be required for the EIN, and you may need demographic updates to link yourself to the Group.RevCycle Partners will...
When can I start the credentialing process?
If you are opening a new practice, or if you are adding a new provider to your practice, the credentialing process can begin 60 days before the practice opens, or 60 days before the new provider starts.If the new hire is a new graduate, they will need their license, insurance, and CAQH set up before the credentialing process can begin.
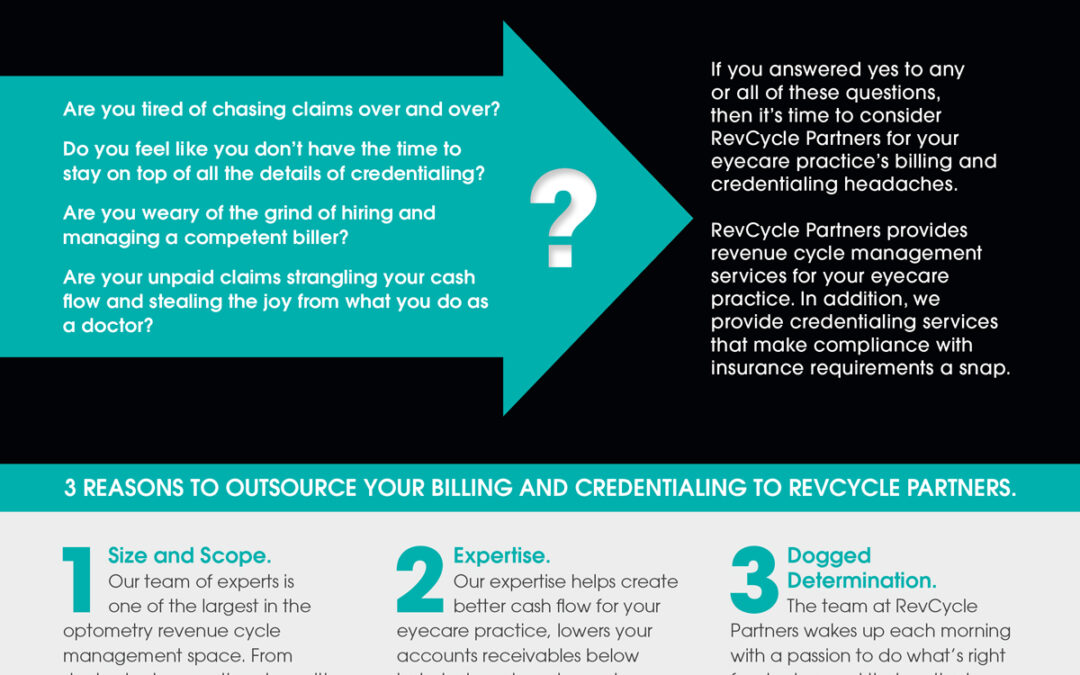
Stop Chasing. Start Collecting.
3 reasons to outsource your billing and credentialing to RevCycle Partners. Are you tired of chasing claims over and over? Do you feel like you don’t have the time to stay on top of all the details of credentialing? Are you weary of the grind of hiring and managing a competent biller? Are your unpaid claims strangling your cash flow and stealing the joy from what you do as a doctor? Download the PDF »
Does RevCycle Partners review claims prior to submission?
RevCycle will scrub claims prior to submission. Some examples of things your biller will look at: adding necessary modifiers, diagnosis for medical necessity based on service code and payer, and cataract co-manage claims for surgeon information and billing details.
How does RevCycle Partners handle transfers?
RevCycle will transfer necessary patient responsibility based on insurance processing: deductibles, co-insurance and copays. RevCycle will provide as much detail as possible using transfer reasons to describe why a transfer was done and why a patient may owe you money.
What if a claim is denied?
If a claim is denied, RevCycle Partners will investigate the denial and take the appropriate action. We will:• Fix the claim and resubmit. RevCycle Partners will file any appeals as needed, as long as we have the documentation to back it up.• Relay the denial back to the office for review/correction. RevCycle Partners will refile the corrected claim.• Drop the denial amount to the patient with a detailed transfer reason.
How many times and for how long will RevCycle Partners attempt to get a claim paid?
RevCycle Partners will exhaust all avenues available to get a claim paid, including filing appeals, chasing denials, and refiling claims.
Will I be required to sign a long-term contract?
With RevCycle Partners there is no long-term commitment. Our service is a month-to-month. You may cancel at any time. We ask for a 60-day termination notice so we can properly wind down the account and reallocate our resources.
Sometimes my staff forgets to add a procedure performed such as a visual field, is this something RevCycle Partners checks for?
No. That is the responsibility of the doctor or office to make sure all services that are performed are coded and applied to an invoice. RevCycle Partners asks that the office verify this as well as make sure that there is a diagnosis on the claim prior to authorizing it. RevCycle Partners will submit corrected claims if something was missed.
Does RevCycle Partners handle patient questions?
There is a relationship between the office and a patient that RevCycle Partners is not familiar with. Our team doesn't want to risk causing any issues for the office or the patient. If the office has a question about a patient balance, they can send their biller a message and/or call. We are happy to provide further details to help explain why the balance is owed.
I still receive EOBs in the mail. How does RevCycle Partners post those?
For items received in office, we ask that those be scanned to a designated area within your system for review by your biller. This can include EOBs, checks, and requests for records.
Does RevCycle Partners send out patient statements?
Sending patient statements is not included with RevCycle Partners’ billing service. That responsibility remains in-office.
Does RevCycle Partners upload EOBs into my EMR software?
RevCycle Partners does not upload EOBs into the EMR software. EOBs are accessible through the website when needed (or by calling the insurance to resend).
Are there any set-up or cancellation fees for the billing service?
There are not any set-up or cancellation fees for RevCycle Partners’ billing services.
Does RevCycle Partners monitor to see if we are getting paid according to our contracts for maximum reimbursement?
RevCycle Partners does not ensure that max reimbursement was received. Max reimbursement/fee schedules are specific to each practice and their contract with the payer. RevCycle Partners does not have access to the fee schedules. We follow the EOB, and we will pull up previous processing to review the codes/payments if needed.
Do I need a clearinghouse to utilize your billing service? Does RevCycle Partners provide the clearinghouse?
A clearinghouse is required in order for us to provide our Medical Claims Management service to any practice. We are not a clearinghouse, nor do we supply the clearinghouse. Practices will need to be set up with a clearinghouse. That way, if the practice makes any changes to their billing services, nothing changes with their billing/workflow.
How does RevCycle Partners access our EOBs?
During onboarding, RevCycle Partners will request login access to the clearinghouse and any external payer portal websites so that we can retrieve electronic remits accordingly.
How often does RevCycle Partners file claims, post payments, work denials, etc?
Our standard process is to access and work our accounts once daily, Monday-Friday. We will take care of any filing, payment posting, and denial follow-up on a daily basis.
Testimonial 005
Our previous biller retired so we decided to outsource our billing to RevCycle and couldn’t be more pleased. Our transition was very smooth and we have not experienced any problems. We appreciate the outstanding service provided by RevCycle.
Testimonial 004
Thanks a million times for your compassionate handling of your customers through the COVID pandemic. RevCycle billing services just about saved my life in Feb-March and the WeVerify service has proven extremely useful.
Testimonial 003
I use RevCycle for both medical and vision billing. I learned the hard way and I’ll pay for the peace of mind that my claims are being submitted, and submitted properly and timely.
Testimonial 002
Our RevCycle biller is very professional, accurate, fast and is like a terrier getting every claim processed to the maximum benefit. We are happy to have her as part of our team.
Testimonial 001
The best move I’ve made in 21 years of business was to outsource to RevCycle. It would have saved so many cashflow dips if I’d partnered with them the first 12 years.

iRefract Selects RevCycle Partners as Its Billing and Credentialing Partner
Fast-growing, national chain plans to outsource key functions of its optometry clinics. March 28, 2022 CHICAGO, IL – iRefract, a nation-wide network of best-in-class optometry clinics, has selected RevCycle Partners as its revenue cycle management (RCM) outsourcing partner. An RCM company for the optometric industry, RevCycle Partners will support iRefract’s growing network of eyecare practices with billing and credentialing services. “RevCycle Partners gives us the opportunity to scale our...

RevCycle Partners Now Supports Eye Cloud Pro EHR and Practice Management Software
The revenue cycle management company extends its insurance billing support to optometry practices using Eye Cloud Pro. September 21, 2021 CHICAGO, IL – RevCycle Partners, a revenue cycle management (RCM) company, now supports Eye Cloud Pro, an eyecare practice EHR and practice management software. “It is apparent that Eye Cloud Pro is gaining momentum in the market,” says CEO Paul Hartge. “We are excited to add support for their software to our outsourced insurance billing service and look...

Optometric Management Group (OMG) Collaborates with RevCycle Partners for Insurance Billing and Credentialing
Ohio-based eyecare company looks to streamline its revenue cycle management operations. August 12, 2021 CHICAGO, IL – Optometric Management Group (OMG) announced that it has selected RevCycle Partners as its outsourcing partner for insurance billing and credentialing. OMG currently owns eight Ohio-based locations and has bold plans to acquire more practices in the next few years. Outsourcing its revenue cycle management functions enables OMG to create efficiencies in its operations. “We’re...

Eyefinity and RevCycle Partners Team Up to Offer Billing and Management Solutions
May 17, 2021 RANCHO CORDOVA, Calif. and CHICAGO, Il – Eyefinity®, a VSP Global® company and leader in practice management and electronic health records software, today announced partnership with RevCycle Partners, a leader in revenue cycle management in the optometric industry. The partnership will enable eyecare professionals to focus on patient care by outsourcing services, such as insurance billing and credentialing, through RevCycle Partners. “This partnership is the latest example of our...

RevCycle Partners Now Supports Eyefinity Optometry Practice Management and EHR Software
The revenue cycle management company now supports optometry practices using Eyefinity. November 1, 2019 CHICAGO, IL -- RevCycle Partners, a revenue cycle management company serving eyecare practices, now supports EyefinityPMS, an optometry practice management and EHR software provider, with its insurance billing services. “Supporting Eyefinity is a natural extension of our Officemate support,” says CEO Paul Hartge. “As practices migrate from Officemate to Eyefinity we are excited to be able to...

RevCycle Partners Launches Benefits & Eligibility Verification Service
“WeVerify” provides eyecare practices a complete and instant picture of patient benefits. September 16, 2019 CHICAGO, IL -- RevCycle Partners, a revenue cycle management company for eyecare practices, has launched WeVerify, a comprehensive service that verifies patient benefits and drives new revenue opportunities for the practice. For many eyecare practices, patient benefits verification before the visit is an incomplete process or perhaps not done at all. RevCycle Partners’ WeVerify service...

Cleinman Performance Partners Selects RevCycle Partners as a Referred Vendor
Partnership supports Cleinman objectives of helping private optometry practices grow and succeed. September 16, 2019 CHICAGO, IL – Cleinman Performance Partners, the business development consultancy for larger optometry practices, has selected RevCycle Partners, a revenue cycle management (RCM) company serving eyecare practices, as their referred revenue cycle management vendor. Cleinman works exclusively with larger private practice optometrists, providing solutions for virtually any business...

RevCycle Partners Now Supports Compulink EHR and Practice Management Software
The revenue cycle management company extends its insurance billing support to optometry practices using Compulink. August 1, 2019 CHICAGO, IL -- RevCycle Partners, a revenue cycle management company serving eyecare practices, now supports Compulink, an EHR and Practice Management software provider. “It was important for us to add support for the Compulink platform for our billing services,” says CEO Paul Hartge. We see Compulink in many large practices through the U.S., and we are pleased to...

RevCycle Partners Becomes a Preferred Vendor Partner of PECAA
The partnership strengthens both organizations’ mission to help optometry practices thrive in today’s competitive environment. April 21, 2019 CHICAGO, IL – RevCycle Partners, a revenue cycle management company serving eyecare practices, has become a preferred vendor partner of Professional Eye Care Associates of America (PECAA), one of the premier doctor alliance groups in the U.S. The sponsorship enables RevCycle Partners to provide its expertise in insurance billing and credentialing to...

RevCycle Partners Now Supports Officemate and CrystalPM
The revenue cycle management company positions itself to grow its insurance billing services with the addition of the leading platforms in optometry. April 1, 2019 CHICAGO, IL -- RevCycle Partners, a revenue cycle management company serving eyecare practices, now supports Officemate and CrystalPM, two of the leading practice management and EHR software providers, with its insurance billing services. “By adding support of Officemate and CrystalPM to our existing RevolutionEHR offering,” says...

RevCycle Partners Launches Two New Credentialing Services for Eyecare Practices
Seasoned optometry revenue cycle management team offers tailor-made credentialing services nationwide. January 28, 2019 CHICAGO, IL -- RevCycle Partners, a revenue cycle management company for eyecare practices, recently launched WeCredential, a service for optometrists who seek to outsource their credentialing tasks. WeCredential has two offerings, the first is Managed Services, which focuses exclusively on the ongoing maintenance demands of credentialing. The second, On-Demand, helps...

RevCycle Partners Now Supports Practice Director Practice Management and EHR Software
The revenue cycle management company takes first step in broadening its platform support for its insurance billing services. June 1, 2018 CHICAGO, IL -- RevCycle Partners, a revenue cycle management company serving eyecare practices, now supports Practice Director, a practice management and EHR software provider. “We are pleased to take our first step in our vision to provide broad platform support within the eyecare vertical,” says CEO Paul Hartge. “It is a validation of the strategy we...

RevCycle Partners Spins Out of RevolutionEHR/Rev360 and Forms New Company
The success of the software’s billing service leads executives to form an independent company. May 15, 2018 CHICAGO, IL – RevCycle Partners, a revenue cycle management company serving eyecare practices, has formally separated from RevolutionEHR/Rev360 and become an independent company with separate ownership. In 2013, RevolutionEHR, the leading cloud-based software for optometrists, launched “RevCycle” as an outsourced billing service for its software customers. The meteoric rise of RevCycle’s...









