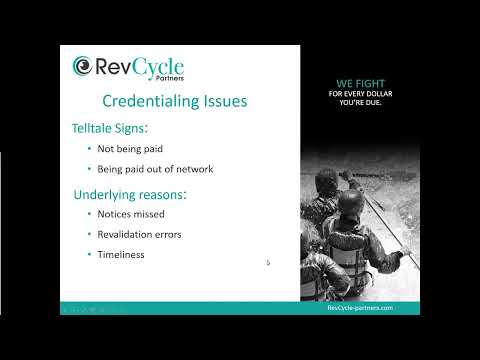
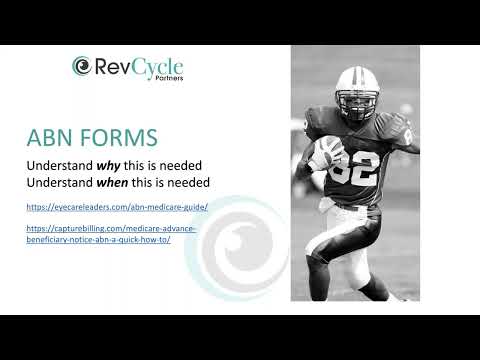
Essential Tips for Eyecare Practices. Credentialing challenges can significantly impact your eyecare practice's revenue and efficiency. This webinar provides insights into avoiding common credentialing mistakes, such as missed notices, revalidation errors, and timeliness issues. Discover strategies for navigating the application process, understanding closed networks, addressing Medicaid-specific requirements, and handling OD-specific concerns. By the end of this webinar, you'll be...