Insurance Billing
Insurance Billing
How to deepen your bench through outsourcing your RCM
How to Deepen Your Bench Through Outsourcing Your Insurance Billing
Does it seem that just when your practice is humming along smoothly you get a staff resignation? Is it difficult to retain insurance billing talent in a hard-to-hire environment? Are you growing faster than you can staff?
There are numerous reasons why you might consider outsourcing your insurance billing.
And you know that who you add to your practice’s billing team makes a significant difference in the financial health of your practice.
You need a deep bench. You need a team singularly focused on insurance billing.
Our large team of US-based eyecare insurance billers are ready to strengthen your team. They are at the top of their game, providing support to hundreds of optometry practices nationwide. Each biller brings with them years of eyecare billing experience plus grit and determination to get claims paid.
All this translates to relief. Relief that comes from receivables being collected on time. Relief that comes from no longer having to hire and train new employees. Relief that comes from better cash flow. Relief that comes from practice efficiency.
We support all major optometry PMS/EHR software and clearinghouses, so we are ready to become part of your team today.
Outsource your insurance billing tasks to RevCycle Partners. Experience the confidence of a deep bench. With our insurance billing service, we do what’s right for you. So you can do what’s right for the patient: provide exceptional patient care.
Are You Wondering if Outsourcing is Right for Your Practice?
There are a lot of questions to consider before making the decision to outsource. Is it worth the effort? Does it make financial sense?
Download this guide for insights on the value of outsourcing.
Learn More about Our Insurance Billing for Optometrists
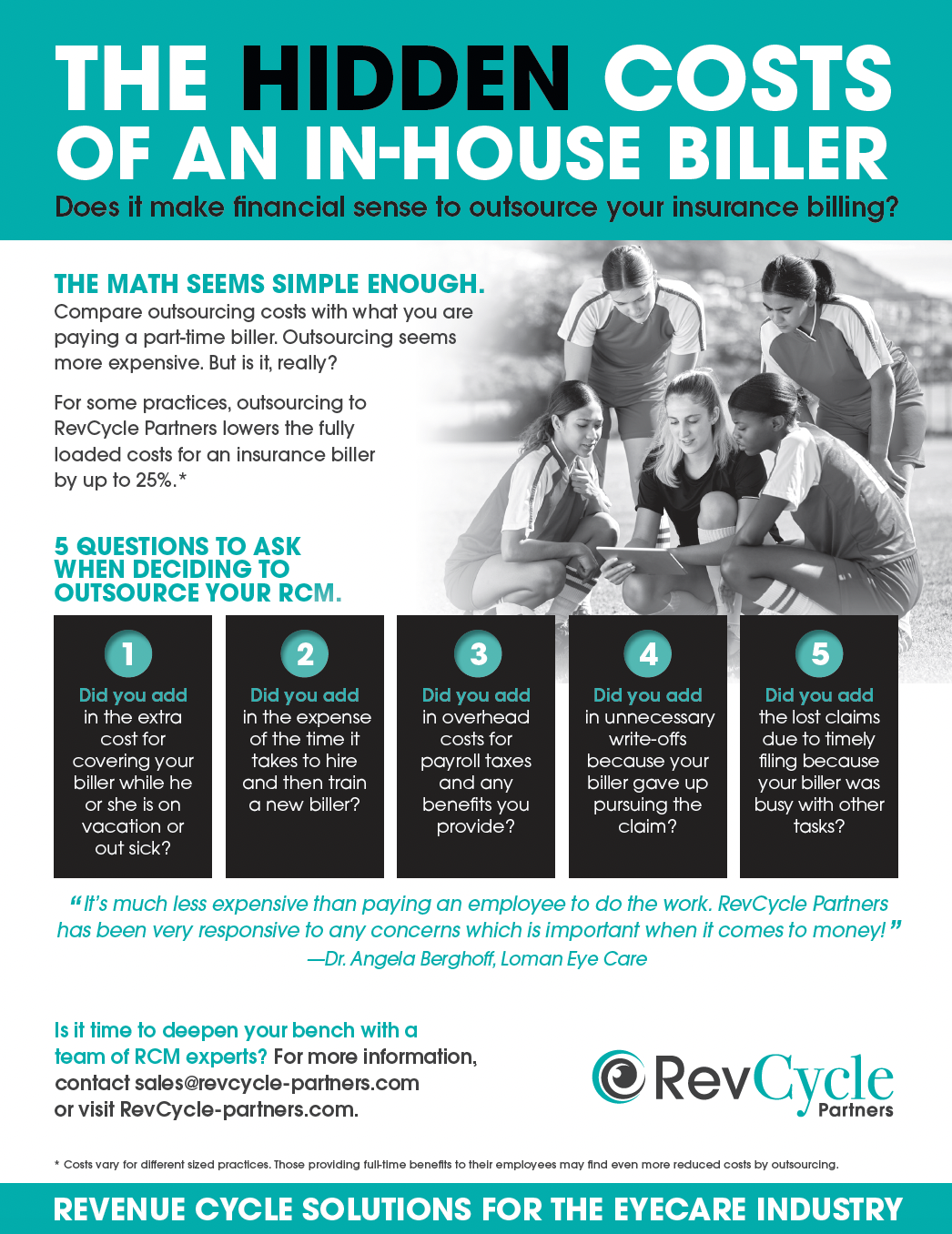
The Hidden Costs of an In-House Biller
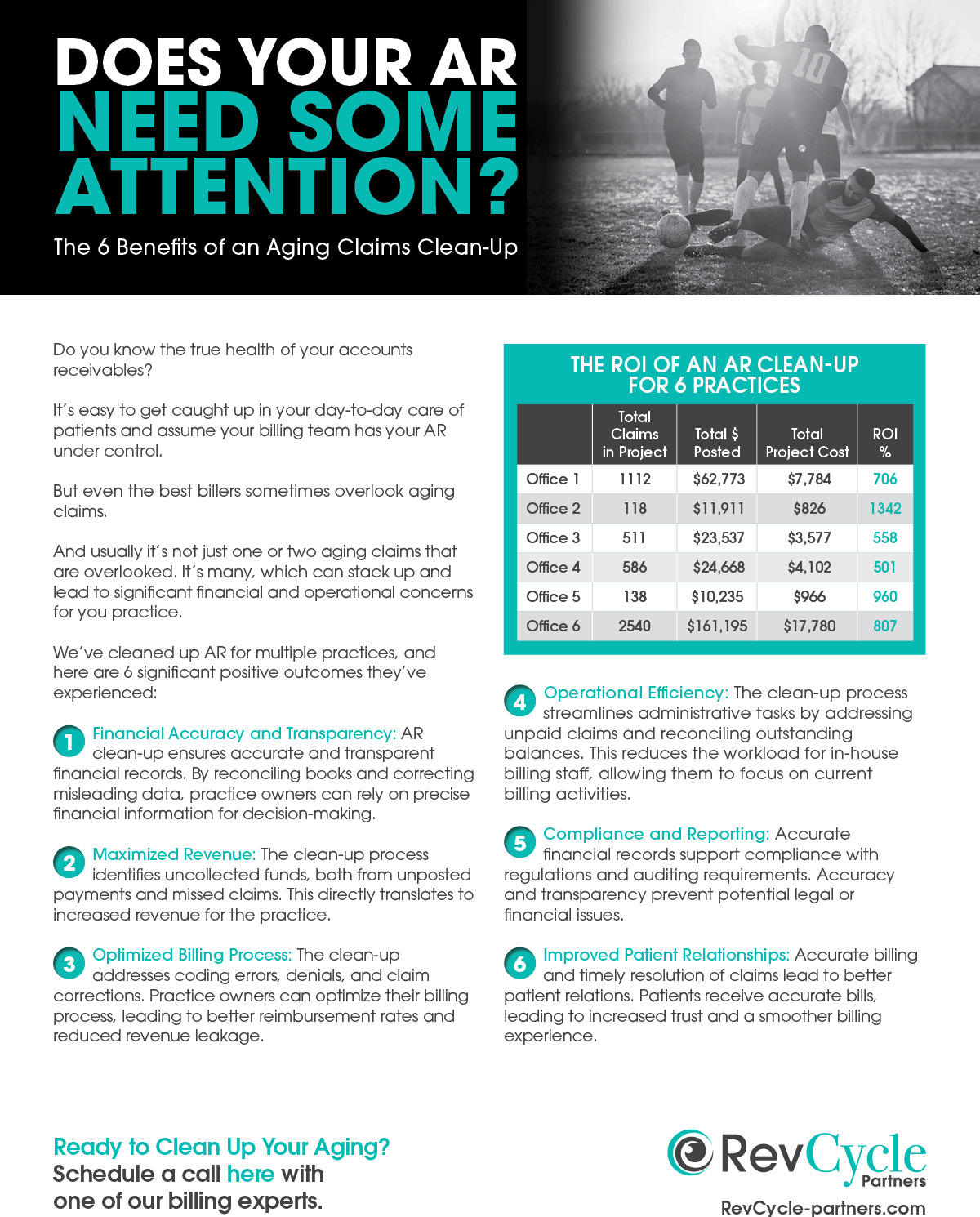
Does Your AR Need Some Attention?
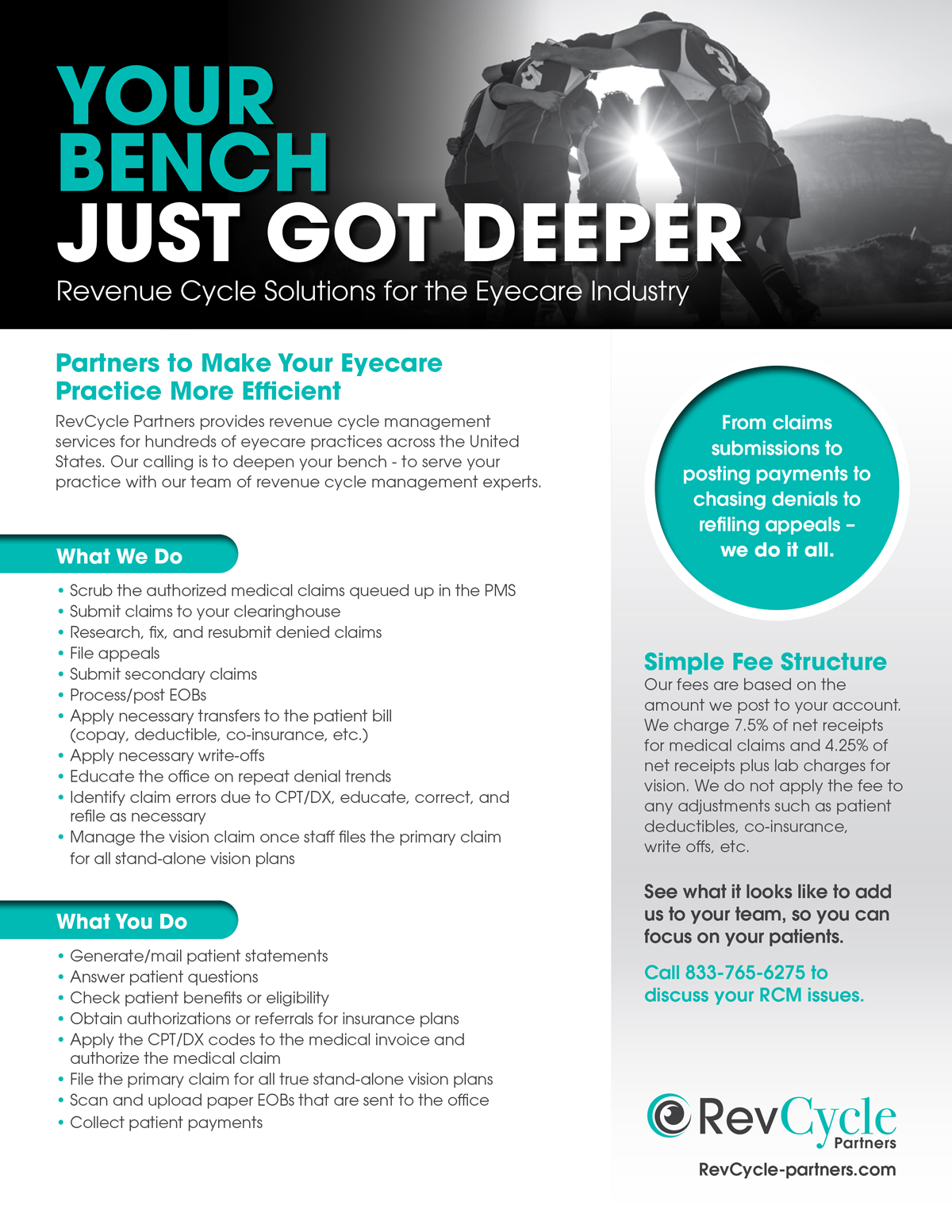
Your Bench Just Got Deeper
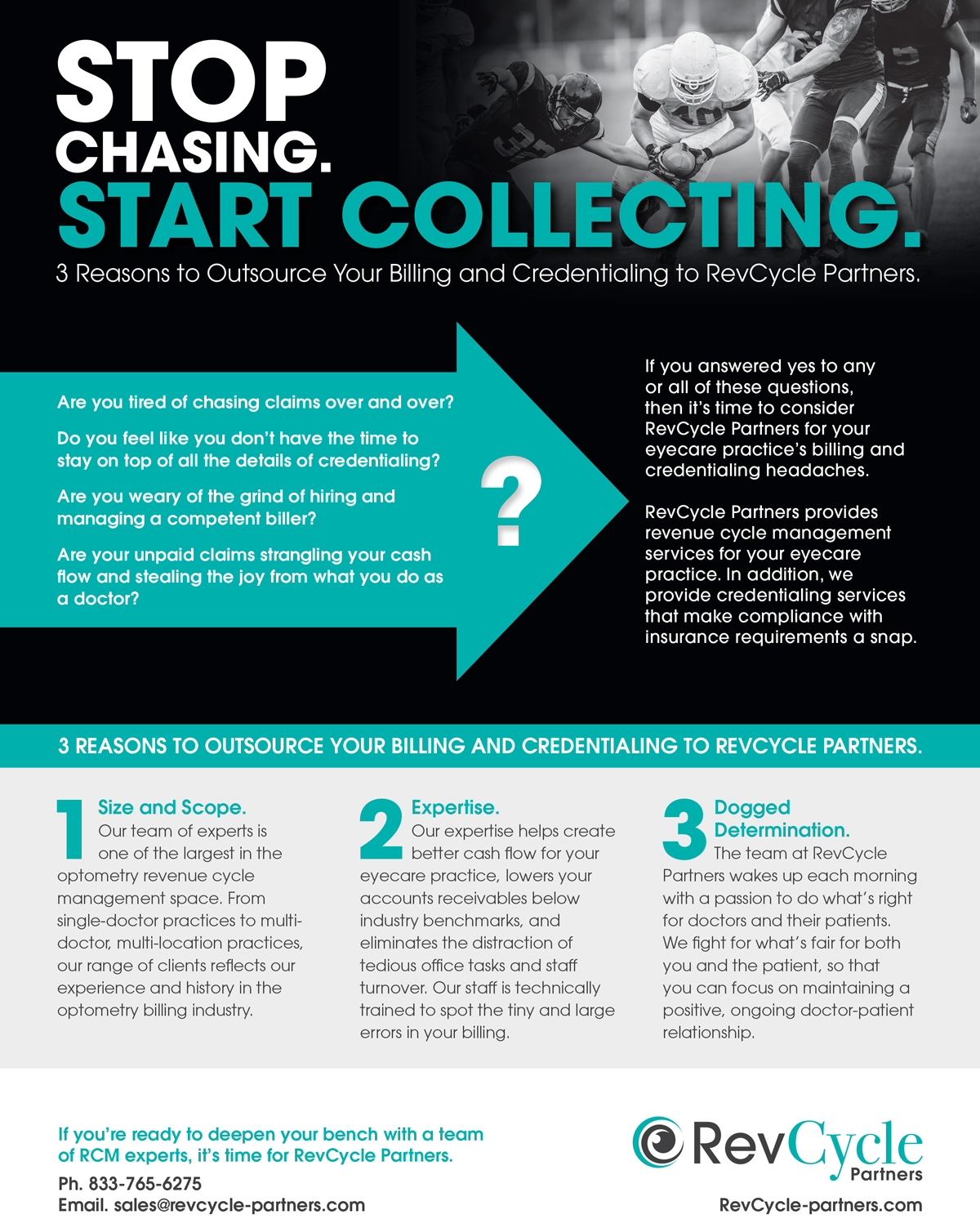
Stop Chasing. Start Collecting.

Avoid Common Credentialing Mistakes

Answering Your Questions about Insurance Billing

How to Navigate Payer Portals

How to Credential a New Provider

How to Simplify Billing for Medicare

Commonly Confused Modifiers

How to Use Modifiers for Insurance Billing

How to Handle Insurance Payer Denials
How to Simplify Billing for Medicare and Medicaid

The Strategic Advantages to Outsourcing Your RCM

The Problems with Keying Vision Claims In-House

Should You Outsource Your Eyecare Insurance Billing?

How Outsourcing Became an Essential Component of a Growing Practice

No-Nonsense HIPAA Compliance

Everything You Need to Know about WeCredential Maintenance Service

A Realistic Timeline for Credentialing Your Optometry Grad

Tune Up Your Eyecare Practice’s RCM Processes

Signs Your Biller Might Not be on Top of AR
Does RevCycle Partners review claims prior to submission?
RevCycle will scrub claims prior to submission. Some examples of things your biller will look at: adding necessary modifiers, diagnosis for medical necessity based on service code and payer, and cataract co-manage claims for surgeon information and billing details.
How does RevCycle Partners handle transfers?
RevCycle will transfer necessary patient responsibility based on insurance processing: deductibles, co-insurance and copays. RevCycle will provide as much detail as possible using transfer reasons to describe why a transfer was done and why a patient may owe you money.
What if a claim is denied?
If a claim is denied, RevCycle Partners will investigate the denial and take the appropriate action. We will:• Fix the claim and resubmit. RevCycle Partners will file any appeals as needed, as long as we have the documentation to back it up.• Relay the denial back to the office for review/correction. RevCycle Partners will refile the corrected claim.• Drop the denial amount to the patient with a detailed transfer reason.
How many times and for how long will RevCycle Partners attempt to get a claim paid?
RevCycle Partners will exhaust all avenues available to get a claim paid, including filing appeals, chasing denials, and refiling claims.
Will I be required to sign a long-term contract?
With RevCycle Partners there is no long-term commitment. Our service is a month-to-month. You may cancel at any time. We ask for a 60-day termination notice so we can properly wind down the account and reallocate our resources.
Sometimes my staff forgets to add a procedure performed such as a visual field, is this something RevCycle Partners checks for?
No. That is the responsibility of the doctor or office to make sure all services that are performed are coded and applied to an invoice. RevCycle Partners asks that the office verify this as well as make sure that there is a diagnosis on the claim prior to authorizing it. RevCycle Partners will submit corrected claims if something was missed.
Does RevCycle Partners handle patient questions?
There is a relationship between the office and a patient that RevCycle Partners is not familiar with. Our team doesn’t want to risk causing any issues for the office or the patient. If the office has a question about a patient balance, they can send their biller a message and/or call. We are happy to provide further details to help explain why the balance is owed.
I still receive EOBs in the mail. How does RevCycle Partners post those?
For items received in office, we ask that those be scanned to a designated area within your system for review by your biller. This can include EOBs, checks, and requests for records.
Does RevCycle Partners send out patient statements?
Sending patient statements is not included with RevCycle Partners’ billing service. That responsibility remains in-office.
Does RevCycle Partners upload EOBs into my EMR software?
RevCycle Partners does not upload EOBs into the EMR software. EOBs are accessible through the website when needed (or by calling the insurance to resend).
Are there any set-up or cancellation fees for the billing service?
There are not any set-up or cancellation fees for RevCycle Partners’ billing services.
Does RevCycle Partners monitor to see if we are getting paid according to our contracts for maximum reimbursement?
RevCycle Partners does not ensure that max reimbursement was received. Max reimbursement/fee schedules are specific to each practice and their contract with the payer. RevCycle Partners does not have access to the fee schedules. We follow the EOB, and we will pull up previous processing to review the codes/payments if needed.
Do I need a clearinghouse to utilize your billing service? Does RevCycle Partners provide the clearinghouse?
A clearinghouse is required in order for us to provide our Medical Claims Management service to any practice. We are not a clearinghouse, nor do we supply the clearinghouse. Practices will need to be set up with a clearinghouse. That way, if the practice makes any changes to their billing services, nothing changes with their billing/workflow.
How does RevCycle Partners access our EOBs?
During onboarding, RevCycle Partners will request login access to the clearinghouse and any external payer portal websites so that we can retrieve electronic remits accordingly.
How often does RevCycle Partners file claims, post payments, work denials, etc?
Our standard process is to access and work our accounts once daily, Monday-Friday. We will take care of any filing, payment posting, and denial follow-up on a daily basis.
Testimonial 027
Testimonial 026
Testimonial 025
Testimonial 024
Testimonial 023
Testimonial 021
Testimonial 020
Testimonial 019
Testimonial 018
Testimonial 017
Testimonial 016
Testimonial 015
Testimonial 014
Testimonial 013
Testimonial 012
Testimonial 011
Testimonial 010
Testimonial 009
Testimonial 008
Testimonial 007
Testimonial 006
Testimonial 005
Testimonial 004
Testimonial 003
Testimonial 002
Testimonial 001
Insurance Billing for Optometrists
RevCycle Partners provides insurance billing for optometrists.
Ready to experience the relief that comes from fewer hiring headaches, better cash flow and receivables that are collected on time?









